- The Problem: The research community and its funders underinvest in studies that explore how to improve disease care and prevention.
- The Solution: Help funders understand that these studies are as innovative and impactful as biomedical discovery.
- Why Now: Biomedical discovery alone is not sufficient to improve people’s health, especially communities who are under-represented and under-resourced.
The Healthcare Challenge
Positive healthcare outcomes depend not just on the quality of a procedure, therapy or drug but on how that service is delivered to patients. A drug might be approved, but are people taking it? Hospitals might offer a service, but are patients willing or able to go there? And will an inefficient or otherwise negative experience with a hospital or healthcare provider prevent patients from continuing to seek care?
These are all vital questions, but often, there’s little available funding to adequately address them. That’s because the medical and scientific research community—along with government and private funders—overwhelmingly spend their energies on developing the medicine itself. The emphasis is on discovery: “Studying the molecular makeup of specific diseases with the aim of making new treatments as opposed to understanding how best to deliver that medicine, so it reaches diverse populations,” says Sindy Escobar Alvarez, DDF’s Program Director for Medical Research. “We also don’t focus nearly enough on studying prevention—how best to keep people from getting sick in the first place.”
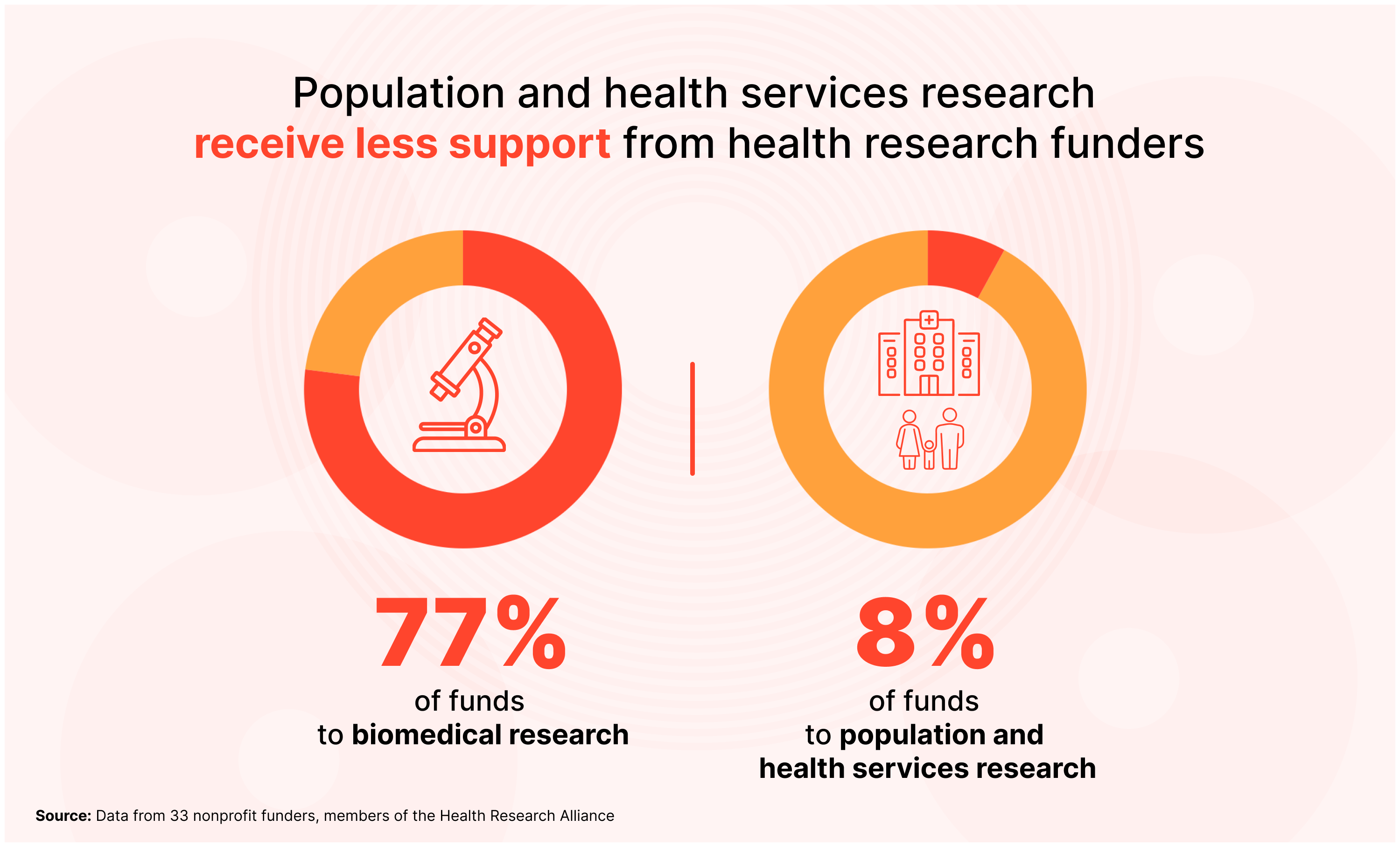
The numbers show the disconnect. Between 2012-2022, 33 nonprofit health research funders directed 77 percent of their funds toward biomedical research, 15 percent for clinical research and just 8 percent for research on population and health services.
What’s Behind this Challenge?
Dr. Ashwin Vasan is a physician, professor of public health at Columbia University and former New York City Health Commissioner. He has some theories about why it’s harder to fund studies that explore the challenges to treatment delivery.
He says biomedical and clinical research is often conducted in “laboratory conditions.” You generate a hypothesis and you set about testing that hypothesis in a highly controlled setting. But research that focuses on prevention, access and delivery, can be much harder to control and to track, especially since it depends on both quantitative metrics, like statistics, and qualitative ones, like in-depth interviews. These studies must often follow populations over long periods of time. (Observational cohort studies like the Nurses or Physicians Health Study is an example.) And this research may elicit associations, but not causality and data on service delivery.
Or take health services research, a multidisciplinary field that explores how systemic social, financial and policy reforms can improve healthcare delivery. Such research can be messy, Dr. Vasan says, because you’re observing “real world conditions,” often in response to a problem that’s unfolding in real time.
Because delivery often intersects with real-world, real-time conditions, paying attention to these problems—and funding solutions—can require public policy action. That’s a lot more complicated than funding a lab or basic clinical research. And as Dr. Vasan explains, the people who are most impacted by poor healthcare delivery tend to be under-resourced communities, so they don’t always have people speaking up for them.
“We face that a lot in healthcare delivery and in public health, particularly when it comes to reaching marginalized groups for whom there isn't natural political and social power and voice,” says Dr. Vasan. “That hurts them when decision-makers and resource allocators are deciding on what gets funded and what does not. Prioritizing their prevention and care delivery needs is too often an afterthought rather than central to the research agenda.”
The Covid Vaccine: A Real-world Example
Covid vaccines encapsulate much of this. As Dr. Vasan explains, when Covid vaccines were first introduced, they were shown to be successful in preventing serious illness and death. But in New York City, older Black Americans, in particular, weren’t leaving their homes to get vaccinated, even though the vaccines were widely available and widely supported as safe and effective.
When public health workers began to study the mechanisms of delivery—how vaccines were advertised and how vaccine education was done, as well as where they were administered and who administered them—they began to understand the disconnect. Many older Black Americans, especially those who lived in public housing, didn’t have stable internet access, and they were afraid to take public transportation during the pandemic. They couldn’t easily make or attend appointments, even at local drug stores. Further, research revealed that practical and historical inequities led older Black Americans to be inherently distrustful of the vaccine and of the public health authorities advocating for it. Successful delivery, and closing the Black-White vaccine gap, required overcoming this trust barrier.
“And so, the NYC Health Department designed an intervention and tested it at the same time,” said Dr. Vasan. “Which is to say, how do we reduce every barrier - social, economic, logistical, and cultural - to entry for these populations to access the vaccine?”
The NYC team began testing new approaches in real time. They started bringing the vaccines to the population in need—advertising and administering it in culturally-trusted spaces where older Black Americans were already going, like barber shops, churches and community centers. They worked with trusted community stakeholders, like Black doctors and pastors to help combat misinformation. They did home-based vaccination for New Yorkers with limited mobility who could not physically leave home. And they invested in local organizations - nonprofits, healthcare facilities, and otherwise - that had a trusted track record of engagement, and hired community health workers tasked to do vaccine education, outreach, and engagement into care, as well as distribution of PPE and addressing basic needs.
And as all of this was happening, researchers were tracking vaccination rates between communities that had received this new approach and those who were still waiting for the rollout. They conducted in-depth interviews with the target population to better understand how the new approach was working.
“Our data not only showed that this program was effective,” said Dr. Vasan, “but it helped us establish a set of principles for how we would do this going forward for more tailored outreach for the mpox vaccine, which was about reaching a marginalized population that had historic and well-founded mistrust of healthcare systems and had experienced discrimination and bias.”
Making Change Happen
We should not have to wait for a public health emergency to convince funders that health services research deserves attention. Covid is a prime example. Had pre-pandemic research allowed public health officials to better understand and design interventions to meet the unique challenges older Black Americans were facing around vaccination, they would have been ready with these delivery strategies much earlier. And as a result, fewer people would have gotten sick. Likely many fewer people would have died. So how to convince funders?
First, public health leaders like Dr. Vasan, would like funders to know that answering real-world implementation questions—like how to disseminate a vaccine—requires as much innovation and creativity as making the vaccine in the first place. “We must increase the habit of funding implementation as part and parcel of dissemination and uptake of both proven and novel prevention and care strategies,” he says. “One can then make the case that the delivery question you're asking is both novel and essential to the success of the intervention.”
He says the funder can then be attached to something that is field-defining or field-shifting in some critical way, even if they did not fund the primary clinical research.
Third, we need to change the conversation around the importance of health services research, so that funders understand how truly vital it is for preventing illness and saving lives. We have seen tremendous scientific and medical advancements, but once those drugs and treatments leave the lab or the clinical study, their adoption will be subject to all kinds of unforeseen real-world conditions.
“There is an assumption in the research community that the best ideas will naturally be adopted, and that effect size will determine the size of political will to make policy and affect change at scale,” Dr. Vasan says. “That is rarely the case. Policy does not work with magic bullets. Rather, it requires a level of discernment on the part of the funder to say, well actually, this is a very important set of questions that have held us back, to-date, and that are deserving of our support, as much as the primary innovation itself.”